This guide combines compassionate, real-world advice with evidence-based guidelines from reputable sources like the American Academy of Pediatrics (AAP), Centers for Disease Control and Prevention (CDC), and La Leche League (LLL). Our goal is to provide a single, super-detailed resource to help you pump with purpose and confidence.
The Foundational Principle: Supply and Demand
Before we dive in, let’s remember the golden rule of milk production: your body makes milk based on supply and demand. When milk is removed from the breast, either by a nursing baby or a pump, it sends a hormonal signal to your brain to produce more. The more frequently and effectively milk is removed, the stronger that signal becomes.
Pumping is a way to artificially create this demand. It’s a powerful tool, but improper timing can lead to issues like oversupply, undersupply, or engorgement. Let’s ensure you’re using it effectively.
When to Start Pumping Breast Milk?
The ideal start time depends entirely on your situation, but the goal is always to establish direct breastfeeding first, whenever possible.
- For most healthy, full-term babies: It is recommended to wait until breastfeeding is well-established, typically around 3−6 weeks postpartum. This allows your supply to regulate based on your baby’s unique nursing cues and reduces the risk of oversupply or bottle preference. Introducing a pump too early without a medical reason can signal your body to produce more milk than needed, leading to painful engorgement or mastitis.
- Immediate Pumping (Medical Exceptions): There are critical situations when you should begin pumping right away.
- If your baby cannot nurse: This includes babies in the NICU, those born prematurely, or infants with medical issues preventing a good latch.
- When to start: Begin pumping as soon as possible after birth, ideally within 1−6 hours postpartum. Evidence shows that mothers who start pumping within one hour of birth have significantly higher milk volumes by the third week compared to those who start at the six-hour mark.
- How to start: Begin with hand expression to collect precious colostrum, then transition to a hospital-grade double electric pump.
General Guidelines for Pumping Frequency and Timing
Once you begin, consistency is key. Your goal is to mimic your baby’s natural feeding patterns.
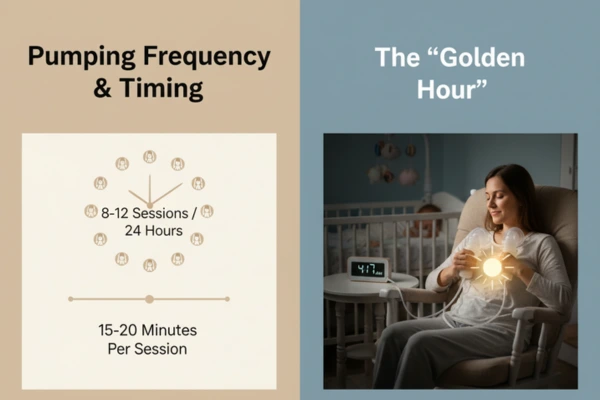
- Daily Frequency: Aim for 8−12 pumping sessions in a 24-hour period for the first few months. This often totals about 120 minutes of pumping per day.
- Session Length: A standard session lasts 15−20 minutes per breast (or 15−20 minutes total if double pumping). Continue pumping for an additional 2−5 minutes after milk flow slows to a trickle. This helps to fully empty the breast and stimulates future production. Watch for multiple let-downs (milk release), aiming for 2−3 per session.
- Best Time of Day: Your milk-making hormone, prolactin, is highest overnight and in the early morning.
- The “Golden Hour” to pump is in the morning, about 30−60 minutes after your baby’s first feed.
- Include an overnight session, ideally between 2−5 AM, to leverage this peak prolactin. Consistently skipping night sessions can lower your overall supply by as much as 20−30%.
- Tracking Output: While every person is different, a typical daily milk volume for a baby aged 1−6 months is 750−1,035 mL (25−35 oz). Do not fixate on this number. Your pump output is not an accurate measure of your worth or your total milk supply; a baby is far more efficient at removing milk than any pump.
Pumping Scenarios: A Detailed Breakdown
Your pumping schedule will change based on your goals. Here’s how to approach different situations.

1. The Early Days & Establishing Supply (0-6 Weeks)
If your baby is nursing well, you only need to pump if medically indicated (as described above) or for brief relief from engorgement (pumping just 2−5 minutes for comfort). Your primary focus should be nursing on cue, at least 8−12 times a day.
2. Building a Stash for Returning to Work or School
- When to Start: Begin pumping about 2−4 weeks before your return date.
- How to Pump: Add one pumping session per day, ideally during the “Golden Hour” after the first morning feed.
- How Much You Need: You only need a small stash! Aim for enough for 2−3 days of separation. A baby typically takes 1−1.5 oz (30−45 mL) of milk per hour you are away. Freeze milk in small, manageable portions (2−4 oz) to avoid waste.
3. Pumping at Work
Once back at work, pump every 2−3 hours you are separated from your baby to match their feeding schedule. For a typical 8-hour workday, this means 2−3 pumping sessions. A hands-free pump can be a game-changer for multitasking.
4. Exclusively Pumping
This is a true labor of love. Treat your pump as your baby.
- Schedule: Pump 8−12 times per day, totaling at least 120 minutes, for the first 3−4 months. Do not go more than 4−5 hours between sessions.
- Feeding the Baby: Use paced bottle-feeding techniques, which mimic the flow of breastfeeding and allow the baby to control the pace of the feeding.
5. To Increase a Low Milk Supply
There are many methods that may help with increasing your milk supply, but here I’m listing some quick ones.
Add Sessions: Pump for 10−15 minutes immediately after every nursing session. This extra stimulation tells your body to make more milk.
Power Pumping: Mimic a baby’s cluster feeding by power pumping once a day for 3−7 days. The schedule is:
- Pump for 20 minutes
- Rest for 10 minutes
- Pump for 10 minutes
- Rest for 10 minutes
- Pump for 10 minutes You should start to see results in 2−3 days.
6. Managing Oversupply and Engorgement
If your breasts are painfully full, pump just enough for relief, not to empty them completely. Pumping to empty will only worsen the oversupply cycle. If you have a chronic oversupply, work with an IBCLC to gradually and safely reduce pumping sessions.
7. Weaning or Reducing Pumping
This must be done slowly to avoid plugged ducts or mastitis.
- The Method: Drop one pumping session every 3−5 days. Start with your least productive session.
- For Comfort: During the transition, if you feel overly full, pump only for a few minutes to relieve the pressure. The entire process may take several weeks.
8. Other Specific Situations
- Travel or Separation: Stick to your baby’s feeding schedule as closely as possible to maintain supply.
- Illness or Medication: Most medications are safe for breastfeeding. If you must take something unsafe, “pump and dump” (pump and discard the milk) to maintain your supply until you can resume nursing.
- Alcohol: The current advice is to wait approximately 2 hours per alcoholic drink before nursing or pumping for your baby.
- Baby’s Growth Spurts: If your baby is nursing more frequently, you do not necessarily need to pump more. However, if you are separated, you may want to add a pumping session to mimic their increased demand.
Tips for Effective and Comfortable Pumping
- Equipment: Use a high-quality double electric pump. Correct flange fit is essential. Your nipple should move freely in the tunnel without rubbing. It should not be painful.
- Techniques: Use “hands-on pumping”—massage and compress your breasts before and during pumping to maximize output. Looking at photos or videos of your baby can help trigger your let-down reflex.
- Safety & Hygiene (CDC Guidelines): Wash pump parts in hot, soapy water after every use. Sanitize all parts daily if your baby is under 2 months old, premature, or has a weakened immune system.
- Milk Storage (CDC Guidelines):
- Room Temperature: Up to 4 hours.
- Refrigerator: Up to 4 days.
- Freezer (Standard): Up to 6−12 months for best quality.
- Always thaw frozen milk in the refrigerator or in a bowl of warm water. Never refreeze thawed milk.
A Final Word of Encouragement
Knowing when to pump empowers you to meet your personal breastfeeding goals. Please remember, the ounces you see in a bottle are not a measure of your success or your love for your baby. You are doing amazing work.
If you ever experience pain, have persistent supply concerns, or simply feel overwhelmed, please reach out to an IBCLC. We are here to provide personalized, judgment-free support for your unique journey.
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with your healthcare provider or a qualified IBCLC for personalized guidance regarding your health and your baby’s care.





